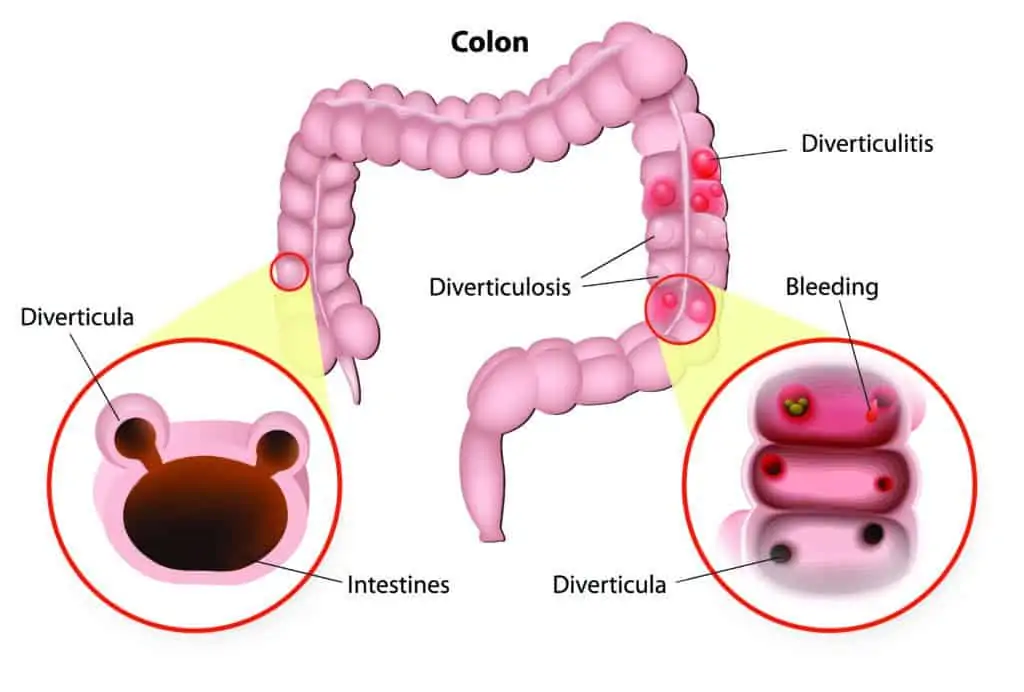
Diverticula are small pouches that bulge out from the intestinal wall at weak points between the muscles. Diverticular disease simply means that a person has multiple diverticula in their gastrointestinal tract.
Diverticula are mostly seen in the lower parts of the large bowel (colon). They are extremely common, with 50% of people over 60 years old having diverticular disease in their colon. Only 20% of people with diverticular disease will develop a complication like diverticulitis.
Diverticular disease is caused by a diet low in fibre, chronic constipation and straining, and age-related weakness of the bowel wall musculature.
The four main problems that may arise from diverticular disease are:
- Inflammation and infection (diverticulitis)
- Bleeding
- Perforation (rupture)
- Abscess formation
Symptoms of diverticulitis (inflammation and infection) include:
- Pain in the lower abdomen (usually to the left side)
- Fevers and/or chills
- Nausea
- Vomiting
- Constipation or diarrhoea
Diverticulitis is diagnosed by a history, clinical examination, blood tests and a CT scan. The treatment will depend on the severity of the inflammation. Sometimes your GP will be able to manage diverticulitis with oral antibiotics. If the symptoms are more severe you may need admission to hospital for intravenous (IV) antibiotics and fluids while the bowel is rested (nothing to eat or drink). You may need to be in hospital for up to five days or more while food is reintroduced gradually.
In severe cases of diverticulitis, the bowel may perforate (rupture) potentially causing peritonitis (a potentially fatal inflammation of the lining of the abdominal cavity). This is a surgical emergency and may require an urgent operation.
If you are admitted to hospital with diverticulitis, Dr Lancashire may arrange for a dietician to talk to you about dietary modification to prevent constipation and further attacks. Dr Lancashire may also recommend that you have a colonoscopy in the months following an attack if you haven’t had one before.