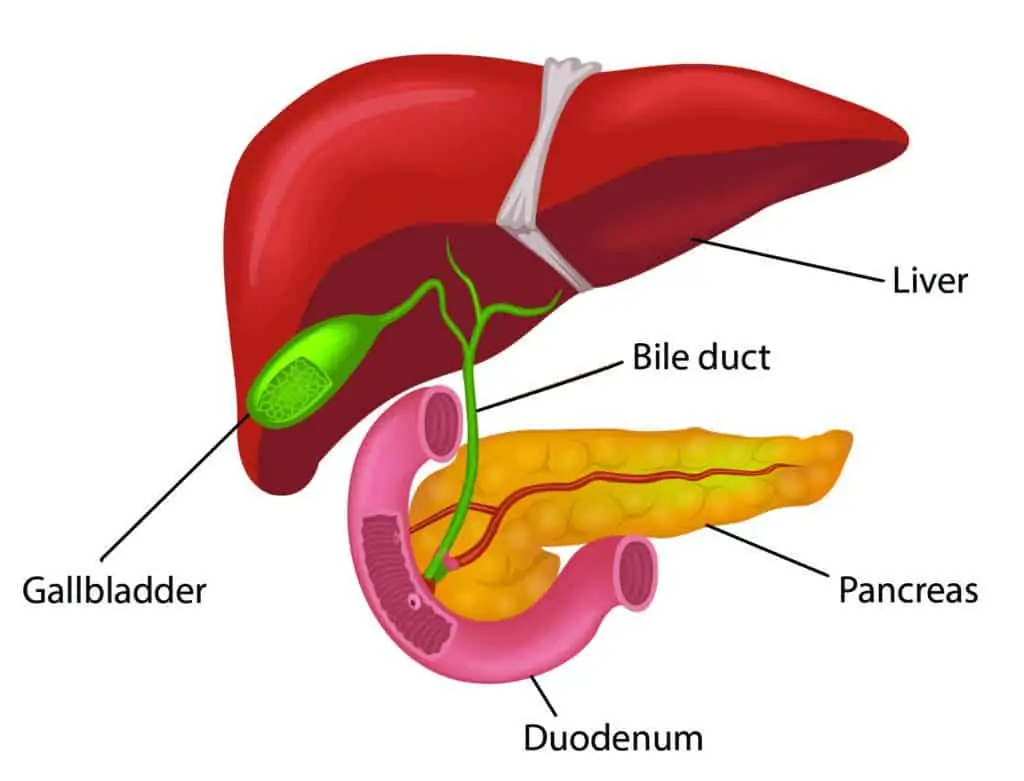
Pancreatitis is inflammation of the pancreas. The pancreas sits in the upper part of the abdomen behind the stomach. It produces hormones insulin and glucagon to control blood sugar levels, and digestive enzymes that break down fats, proteins, and carbohydrates.
The main duct in the pancreas joins the duct that drains bile from the liver and gallbladder (common bile duct) before it empties into the duodenum (the first part of the small intestine).
The pancreas can become inflamed for several reasons. The two most common causes are gallstones and alcohol. Rarer causes include high levels of fat in the blood, medications, trauma (injury), and pancreatic duct divism (duct abnormalities).
Pancreatitis is usually diagnosed on a clinical history, examination, blood tests and x-rays. An ultrasound will look at your gallbladder, pancreas, and ducts from the liver to the bowel. Sometimes a CT scan is required.
The treatment of pancreatitis requires admission to hospital, fasting (nothing to drink and eat), pain relief, and IV fluids until the inflammation settles down. Food is slowly reintroduced as the symptoms improve.
If the pancreatitis is caused by gallstones, you will usually be advised to have your gallbladder removed in a timely manner (see page on gallstones). Sometimes gallstones can get stuck in the end of the bile duct where it meets the pancreas, and you may need a procedure called an ERCP (Endoscopic Retrograde Cholangiopancreotography) to remove it or them. If your pancreatitis is due to alcohol, then it will be recommended that you abstain from alcohol for life.
Pancreatitis can vary in severity from very mild, requiring monitoring in a hospital ward, to critical, requiring admission to an intensive care unit.